The most common mental illnesses

Who is affected by mental illness?
Mental illness affects everyone. It is very common and anyone can develop one, regardless of age, gender, ethnicity or socio-economic status.
Key facts :
- One in two people will experience a mental illness in their lifetime.
- In Canada, approximately 20% of adults have a mental illness.
- All Canadians are indirectly affected by mental illness.
- Less than half of those with a mental illness see a professional for it.
- Mental illness accounts for five of the top ten causes of disability worldwide.
What is mental illness?
Mental illness affects a person’s mind (or brain), just as physical illness affects the body. It causes the person to think, feel and act differently than a person who does not have a mental illness.
For example, the person may be sad or angry for no reason, have incoherent speech or thoughts or experience a lot of anxiety. Some of these behaviours may seem strange or inappropriate: the person may be irritable, agitated and even aggressive for no apparent reason. Mental illness can often lead to physical symptoms, including severe fatigue, loss of appetite, nausea or dizziness. Although the person may notice that something is wrong, the confusion caused by their mental illness and not knowing what to do to improve their situation may prevent them from doing anything about it.
Fortunately, there are various types of support available for people with mental health problems. They can live happy, fulfilling lives.
How do normal emotions and a mental illness differ?
Everyone can feel sad, lonely, depressed, stressed or scared at times. You may feel discouraged, that no one understands you or that things are too difficult to handle. These emotions are a normal part of life. When a person has a mental illness, these emotions may become more intense and last longer than usual, affecting the person’s ability to function as they normally would in many areas of their life (e.g., work, family and social life). People with a mental illness may find it very difficult to get out of bed in the morning, make dinner or take their children to school. They may also have difficulty functioning at work.
- Mental illness affects a person’s thoughts, behaviours and emotions.
- Mental illness is not a sign of weakness or lack of intelligence.
- Mental illness is not caused by a single factor (e.g., genetics or a stressful experience). It develops due to a combination of risk factors.
What causes a mental illness to develop?
It is not yet clear why some people develop a mental illness while others do not. There are usually many possible causes and they vary from person to person. Mental illness usually occurs as a result of a combination of factors related to an individual’s characteristics, family, environment, culture and lifestyle.
A mental illness cannot be caused by ONE specific factor and those affected are not to blame.
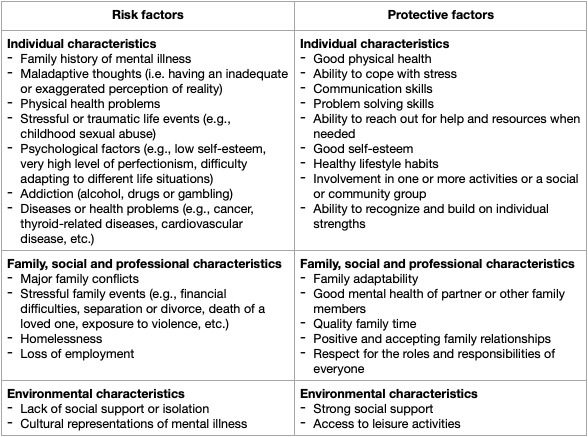
- Certain characteristics increase the likelihood of developing a mental illness : these are called risk factors.
- Other characteristics reduce a person’s risk of developing a mental illness and promote good mental health : these are called protective factors.
Some risk and protective factors cannot be changed (e.g., past events or heredity, i.e., the fact that other people in a person’s family have or have had a mental illness), but others can, such as our thoughts and behaviours in response to a situation. Some protective factors also relate to individual characteristics, which may manifest as different skills and abilities. It is important to recognize these positive characteristics, as they are strengths that help us better cope with life’s challenges and manage everyday stress in a more positive way.
Some examples of risk and protective factors
What are the most common mental illnesses?
The following sections describe the most common mental illnesses observed in the general population. Each mental illness has its own specific characteristics. The way a mental illness manifests can vary from person to person, as each person is different. For example, a person experiencing a depressive disorder may lose their appetite or feel like eating all the time. A person may also have several illnesses at the same time (e.g., a depressive disorder and an anxiety disorder) or different illnesses over the course of their life (e.g., an anxiety disorder, then a depressive disorder). Those with a mental illness may also have substance abuse problems (e.g., alcohol or drug abuse) or, conversely, substance abuse problems may cause a person to develop a mental illness.
Depressive disorder
Being depressed is different than feeling sad from time to time. People living with a depressive disorder often feel hopeless, tired, lonely or exhausted for long periods of time. They often have little energy to do what they need to do – this sometimes even includes getting out of bed or eating. They may sleep all day and lose interest in the things they used to love. They may also feel stressed, irritable, angry or sad for no apparent reason. For example, a parent may sometimes feel depressed after having a child, which is called “postpartum depression.” This can make it difficult for them to take care of the baby and their other children.
“Especially the fatigue. I was very tired and it showed. I had less interest and energy for doing activities. I did the bare minimum. When my children wanted to do an activity, I did it, but it required a lot of energy. I felt guilty about not being able to be there and be a real father to them, and that’s hard too. Of course, they found it a bit disappointing, in a way, to see their father struggle with his feelings and wonder why daddy doesn’t play with them much anymore.” -Daniel, a parent living with a depressive disorder
Bipolar disorder
People with bipolar disorder typically experience dramatic shifts in their moods. They may at times feel very sad, irritable and lacking in energy and at other times be very energetic, overexcited and unable to calm down. During these periods, they may have difficulty sleeping, make expensive purchases, cook or clean in an excessive manner or talk incessantly, for example. They may also feel anxious and have difficulty concentrating.
“When Mom’s not taking her medication correctly, she has ups and downs. Like she’ll go on a manic high and be really dramatic, or she’ll get depressed and tired. So it can be tough to try and talk with her. It gets really confusing because one day she will be fine, but the next day she will burst out crying.” -James, 14*
Anxiety disorders
People with an anxiety disorder experience more intense and frequent worries and fears than people without the disorder. They may continually worry about things that seem unimportant to others. The severe anxiety they feel does not go away even when the situation causing the worry returns to normal. This causes those affected to feel distress. When fears become excessive, persistent and overwhelming, people tend to avoid situations where they may be confronted by their fears, and thus have difficulty doing normal everyday things. For example, someone with a social phobia may avoid eating in public for fear of dropping food and looking ridiculous, or if a person has a specific phobia about dogs, they may not go outdoors to avoid coming into contact with one.
“My mother has always been afraid that something bad would happen: that my father would have an accident, that we wouldn’t do well in school or that we would get sick. She tries not to show it, but we can tell. She’s always a bit defensive. She often calls my dad at work to make sure he’s ok and pressures us to get good grades. Even when we get A+s, she still worries. It’s a little discouraging sometimes.” -Audrey, 17*
- People who experience depression lack willpower.
- People with an anxiety disorder are weak.
- People with bipolar disorder are difficult to manage.
- People with a psychotic disorder have multiple personalities.
Post-traumatic stress disorder
People with post-traumatic stress disorder often feel tired, scared or panicked, or react to things that may seem trivial to others. The disorder can develop in people who have experienced a traumatic event (e.g., a traffic accident, natural disaster or physical or sexual assault). The trauma experienced during these events is often relived through flashbacks and nightmares. These symptoms have a significant impact on their daily lives.
“My dad hasn’t really been himself since he had his car accident six months ago. He is always on edge, like he’s afraid something will happen. He’s pretty grouchy because he doesn’t sleep well and never wants to leave the house anymore. It’s not his fault thought, and I keep reminding myself that.” -Alex, 15*
Obsessive-compulsive disorder
People with obsessive-compulsive disorder are often overwhelmed by uncontrolled and repetitive thoughts that become obsessions (e.g., fear of forgetting to lock the door or fear of catching a disease). Even though they often know that these obsessions are exaggerated, they can’t stop thinking about them. They feel compelled to repeat specific actions to get the obsession off their mind. These actions are called compulsions. They may be clearly related to the obsession (e.g., repeatedly checking that the door is locked if they think they may have forgotten to do it or washing their hands several times if they have obsessions about contamination) or they may not be (e.g., turning the light on and off seven times in a row when they fear their loved one has cancer). They often think that something horrible might happen if they don’t perform their rituals (e.g., that their loved ones will actually be diagnosed with cancer). They may experience a great deal of psychological distress because their obsessions and compulsions take up so much time and can interfere with their daily activities.
“Sometimes we are really late for school because my mom has to check several times to make sure the oven is turned off and that there are no problems with the electrical outlets before we can leave the house. She gets pretty on edge and doesn’t like going out much now unless she has to.” -Jennifer, 13*
Personality disorders
People with a personality disorder exhibit personality traits that can be described as “rigid.” These traits may cause difficulties in functioning (especially on an interpersonal level) and cause suffering for the people concerned and those around them. There are different types of personality disorders, including borderline personality disorder, narcissistic personality disorder, antisocial personality disorder and schizoid personality disorder.
Borderline personality disorder
People with borderline personality disorder often have difficulty managing their emotions and maintaining meaningful relationships with others. They may experience significant mood swings and an intense fear of losing loved ones and seek constant reassurance. They may have sudden outbursts of anger, try to harm themselves or feel frightened or as if they are “losing control.” People sometimes say it’s a bit like being on a roller coaster minus the fun. Their behaviours are often not understood and may stem from a strong sense of fear, loneliness and despair.
“My mom can be really sad and angry sometimes. I remember walking home from school and wondering what mood my mother would be in. Some days we get along like best friends, and others it’s like I can’t do anything right. She gets angry with me for no reason. During these times, I know she can be prone to using substances and hurting herself.” -Marie-Ève, 15*
Narcissistic personality disorder
People with narcissistic personality disorder tend to see themselves as very important, unique and superior to others and may overestimate their abilities, talents and accomplishments. They often believe they are entitled to certain rights or privileges and expect preferential treatment from others. They also believe the only people who can truly understand them are those they deem special and on their level. They may display attitudes or behaviours that others consider arrogant, presumptuous and conceited. In general, they have a strong need to be admired and envied by others and are often obsessed with dreams of grandeur (e.g., unlimited success, power, influence, intelligence, beauty and love). They are therefore very competitive and ambitious. People with this disorder may have difficulty empathizing with others.
Antisocial personality disorder
People with antisocial personality disorder tend to show disregard for the feelings and rights of others. They can be irritable, reckless and aggressive, which can lead to conflicts, fights or physical aggression. They often find it difficult to follow social norms and obey laws. People with antisocial disorder tend to deceive, lie or defraud for material gain or personal gratification, among other things. They often show disregard for their own safety or the safety of others and the consequences of their actions. As a result, they often do not feel remorse, empathy or guilt for their behaviours (e.g., after hurting, abusing or stealing from others) and try to find ways to excuse and/or justify themselves. They may also have difficulty finding a job or satisfying their obligations and commitments. They may also be impulsive and have difficulty planning and organizing ahead of time.
Schizoid personality disorder
People with schizoid personality disorder may show little interest in social and romantic relationships. Generally, they have difficulty developing social ties and prefer to be alone, including during leisure activities. They typically do not seek or value close relationships with others, including their family members. Therefore, they have few, if any, close friends or confidants, except for a relative in some cases. They may also have difficulty emotionally interacting and show a limited number of facial, body or linguistic expressions when interacting with others. As such, it can be difficult for them to empathize, put themselves in someone else’s shoes and understand and express their own emotions. They may also seem indifferent to praise or criticism, other people’s views or demonstrations of affection.
Psychotic disorders
People with a psychotic disorder have difficulty thinking clearly and perceiving reality. When a person loses touch with reality, they may see or hear things that are not really there (hallucinations) or have ideas that are not shared by other people (delusions). For example, they may believe that someone is trying to hurt them or someone close to them. This can be frightening for both the person with the illness and their loved ones, especially if they don’t know they have a mental illness. Schizophrenia is one of the most common psychotic disorders. People with this disorder have difficulty functioning in everyday life because their thoughts, emotions and behaviours are disconnected from reality.
“My father heard voices, didn’t maintain his hygiene, didn’t leave the house and sometimes talked to himself. He stopped working and often slept during the day but stayed awake at night during his delusions. He thought he was being watched and listened to by agents. It was hard. He was hospitalized, and I had to move in with my mother.” -Alexis, 17*
Eating disorders
People with eating disorders are often plagued by thoughts about food, weight or body image. These thoughts go well beyond simple dieting. Some may deliberately choose to limit their food intake (anorexia nervosa); others may eat a large amount of food over a short period and make themselves vomit, take laxatives or exercise a lot to compensate (bulimia); others may overeat, often without adopting compensatory behaviors (binge eating). Those affected may go to great lengths to hide their disorder and may diet constantly, find excuses not to eat, avoid social situations that involve eating or work out excessively. They may spend a lot of time worrying about their body image and feel depressed, anxious or irritable.
“My mom often pretends to eat pieces of her food, but she discreetly gives them to my little brother. She hates being asked if she has eaten. The thing is, she’s already so skinny. She doesn’t see herself as she is.” -Kim, 12*
“I have lived my whole adult life with an eating disorder that I tried to hide from my husband, children and friends, and it was very isolating.” -Adela, a parent living with an eating disorder
A big thank you to Stephanie and Adela, parent members of the LaPProche advisory committee, for their collaboration and involvement in the developing of this fact sheet.
This content was developed at the Université du Québec en Outaouais by the Research and action laboratory for people with mental health problems and their loved ones (LaPProche) with funding from the Fonds des services aux collectivités (FSC2018-013) of the Ministère de l’Enseignement Supérieur and in collaboration with CAP santé mentale.
The information contained in this sheet does not replace seeking professional advice. If you have any questions or concerns, please see a professional.
* Testimonials accompanied by a star were taken from the “When your parent has a mental illness” guide (AICAFMHA, 2014).
References
Fondation Douglas. (2020). Faits sur la santé mentale au pays. https://fondationdouglas.qc.ca/la-sante-mentale/
Gouvernement du Québec. (2020). Conseil et prévention : Santé mentale. https://www.quebec.ca/sante/conseils-et-prevention/sante-mentale/
Gouvernement du Québec. (2020). Problème de santé mentale : Maladie Mentale. https://www.quebec.ca/sante/problemes-de-sante/sante-mentale-maladie-mentale/
Institut universitaire en santé mentale Douglas. (2012). Infos : Santé mentale. http://www.douglas.qc.ca/info_sante
Piché, G., Villatte, A., & Habib, R. (2019). Programme FAMILLE+. Manuel du parent [document inédit]. Université du Québec en Outaouais : Laboratoire de recherche et d’actions pour les personnes ayant des problèmes de santé mentale et leurs proches (LaPProche).
Piché, G., Villatte, A., Habib, R., & Vetri, K. (2019). Programme FAMILLE+. Manuel de l’enfant [document inédit]. Université du Québec en Outaouais : Laboratoire de recherche et d’actions pour les personnes ayant des problèmes de santé mentale et leurs proches (LaPProche).
CAP santé mentale. (2020). S’informer : Archives des capsules Web. https://www.capsantementale.ca/sinformer/videos/
The Children of Parents with a Mental Illness national initiative. (2016). Understanding your mental illness. http://www.copmi.net.au/parents/parenting-with-a-mental-illness/understanding-mental-illness
Villatte, A., Piché, G., & Habib, R. (2020). Quand ton parent a un trouble mental. Conseils et témoignages de jeunes. Université du Québec en Outaouais : Laboratoire de recherche et d’actions pour les personnes ayant des problèmes de santé mentale et leurs proches (LaPProche).
To cite this document, please provide the following reference: LaPProche Laboratory. (2021). The most common mental illnesses. Université du Québec en Outaouais.
© LaPProche 2021| lapproche.uqo.ca
All rights reserved.
Any reproduction in whole or in part by any means whatsoever is prohibited without the written permission of LaPProche.